Hispanics and Diabetes: A Growing Health Challenge
Diabetes is one of the most pressing health concerns facing the United States, and its impact is felt more acutely in certain populations. Among Hispanics, the prevalence of diabetes is significantly higher than in non-Hispanic white populations, which has led to widespread concern among healthcare professionals and community leaders. Understanding the reasons behind this disparity, its consequences, and how to address it is vital for improving the health outcomes of Hispanics in the United States.
Understanding Diabetes
Diabetes is a chronic condition that affects how the body processes blood sugar (glucose). There are several types of diabetes:
- Type 1 diabetes, an autoimmune disorder, occurs when the pancreas produces little or no insulin
- Type 1.5 latent autoimmune diabetes in adults. is a type of diabetes that starts in adulthood and slowly gets worse over time. Like type 1 diabetes, LADA happens when the pancreas stops making insulin.
- Type 2 diabetes, which is far more common, occurs when the body becomes resistant to insulin or doesn’t produce enough to maintain normal blood glucose levels.
Type 2 diabetes is particularly prevalent among Hispanics, and it’s often linked to lifestyle factors like diet, exercise, and weight. High blood sugar levels over a prolonged period can lead to severe complications such as heart disease, kidney failure, nerve damage, and even blindness. Early detection and proper management are critical in preventing these complications.
Prevalence of Diabetes Among Hispanics
According to the Centers for Disease Control and Prevention (CDC), Hispanics are at a significantly higher risk of developing diabetes compared to non-Hispanic whites. In fact, Hispanics are 50% more likely to be diagnosed with diabetes. This statistic is alarming and highlights the disproportionate burden this community bears when it comes to managing this chronic condition.
The reasons for this higher prevalence are multifaceted and include genetic, socioeconomic, and cultural factors. Studies have shown that Hispanics tend to have a genetic predisposition to diabetes, which means they are more likely to develop the disease even when controlling for other factors. However, environmental factors such as diet and access to health care also play a crucial role.
The Role of Genetics
While lifestyle factors are significant contributors to the higher rates of diabetes in Hispanics, genetics also play an essential role. Studies have shown that certain populations, including Hispanics, have a genetic predisposition to insulin resistance and obesity, both of which are major risk factors for developing Type 2 diabetes. This genetic component makes it even more crucial for those at risk to be vigilant about their health and adopt preventive measures, such as maintaining a healthy diet and engaging in regular physical activity.
Complications of Diabetes in the Hispanic Population
Hispanics not only have higher rates of diabetes, but they also tend to experience more severe complications from the disease compared to non-Hispanic whites. These complications include:
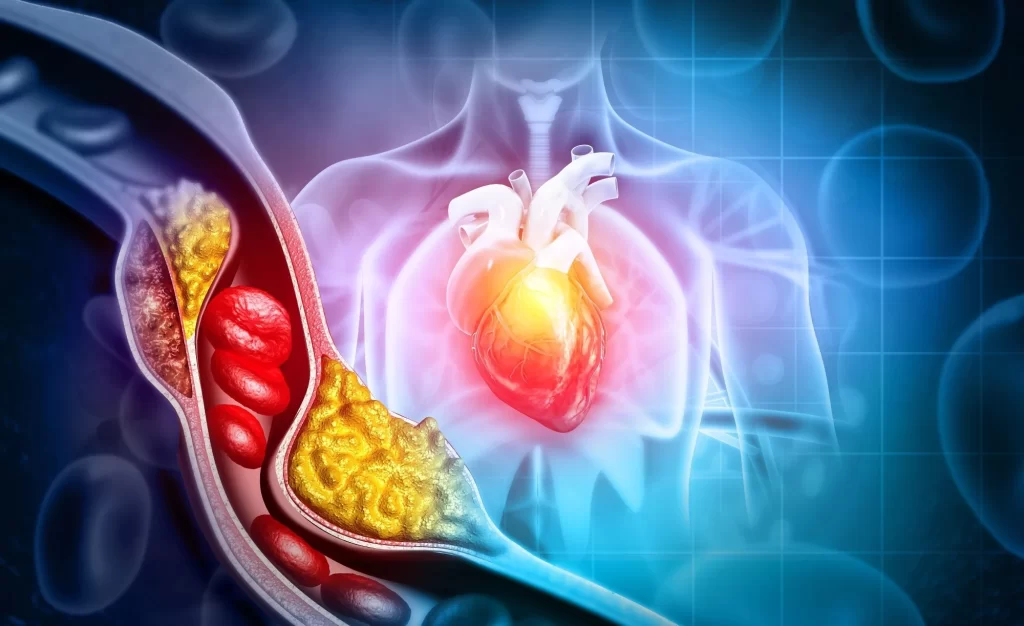
Cardiovascular Disease:
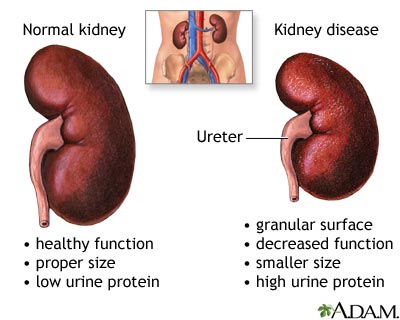
Kidney Disease:
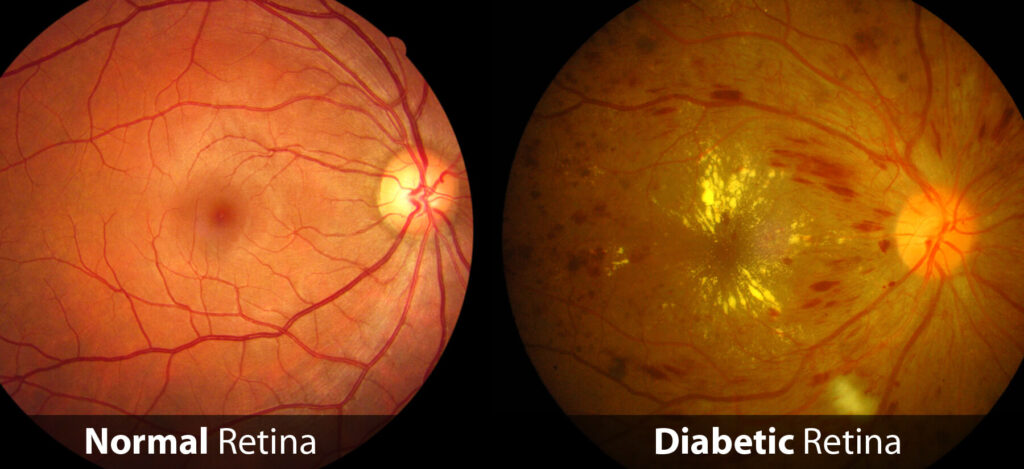
Vision Loss:
Amputations:

Diabetic Skin Changes

Addressing the Diabetes Epidemic Among Hispanics
1. Education: Education is one of the most powerful tools in preventing and managing diabetes. Healthcare professionals must work with community organizations to provide culturally tailored educational programs that teach Hispanics about the risks of diabetes and how to manage the disease. This includes education on nutrition, exercise, and the importance of regular medical checkups.
2. Improved Access to Healthcare: Expanding access to healthcare for underserved Hispanic communities is crucial for early diagnosis and proper diabetes management. Community health clinics that offer bilingual services and culturally competent care can make a significant difference in addressing the healthcare needs of this population.
Conclusion
The high prevalence of diabetes among Hispanics is a significant public health concern that demands immediate attention. While genetic predisposition plays a role, the influence of socioeconomic and cultural factors cannot be overlooked. Addressing this issue will require a comprehensive strategy that includes education, improved healthcare access, and community support. By working together, healthcare professionals, policymakers, and community leaders can make strides in reducing the impact of diabetes on the Hispanic population and improving health outcomes for future generations.
In the future months, we will further discuss diabetes as it affects three different lives.