Maria’s Story – Gestational Diabetes (Mexico)
Our Patient:
Patient: Maria, 32 years old
Location: Mexico City, Mexico
Diabetes Type: Gestational Diabetes
Background:
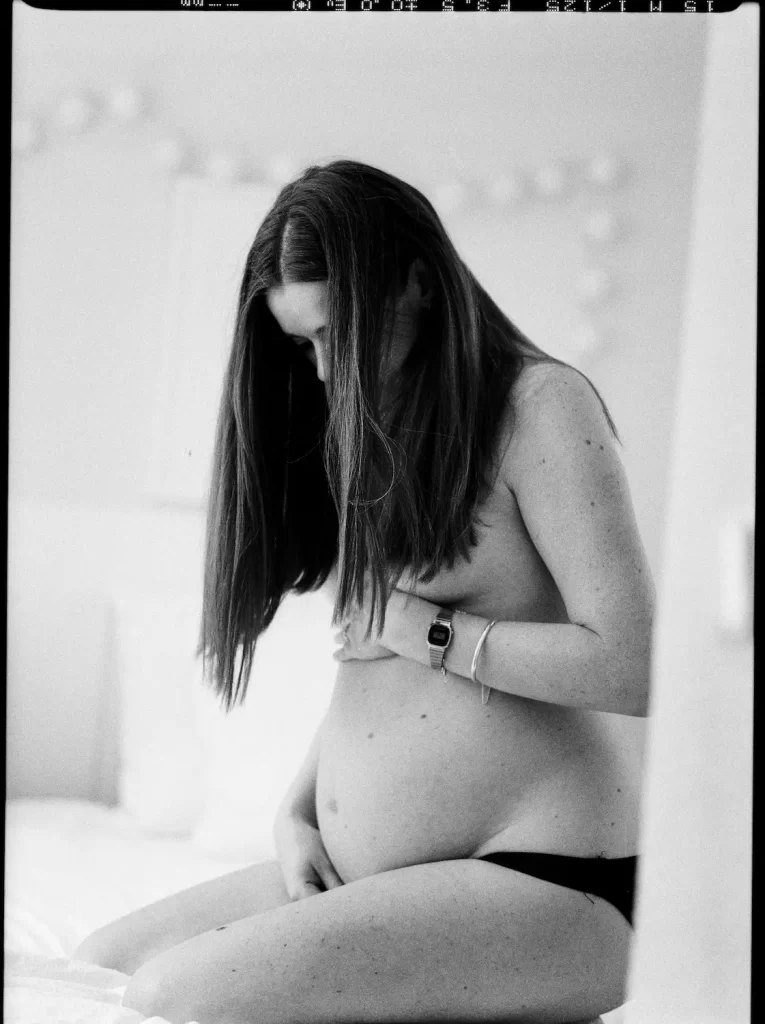
Maria is a 32-year-old woman from Mexico City, pregnant with her second child. During her first pregnancy, everything went smoothly, but this time, Maria began to feel more fatigued than she had before. She initially thought it was just part of the natural demands of pregnancy, especially while managing a household and caring for her 5-year-old daughter.
At her 24-week check-up, Maria’s routine glucose screening revealed elevated blood sugar levels. Her doctor ordered a follow-up glucose tolerance test, which confirmed that she had gestational diabetes. She was caught off guard because she had no prior history of diabetes and felt like her diet hadn’t changed drastically.
Presentation of Symptoms:
Maria’s symptoms were subtle and easy to overlook, especially during pregnancy. She felt thirstier than usual and experienced more frequent urination, but these symptoms are often dismissed as typical of pregnancy. However, when combined with her increased fatigue and unexplained weight gain during the second trimester, the diagnosis made sense
At her next pregnancy visit, her A1c levels and glucose were tested, and the result showed a reading of Aic – 7.6% and glucose 190mg/dl, confirming that she had gestational diabetes. Rosa was shocked, but the signs had been there all along.
– Key Symptoms:
- Increased thirst (polydipsia)
- Frequent urination (polyuria)
- Fatigue beyond typical pregnancy levels
- Rapid weight gain during the second trimester
Diagnosis & Treatment:
Maria was advised to start monitoring her blood sugar at home and work with a nutritionist to manage her diet. Her doctor explained that gestational diabetes can lead to complications if left unmanaged, both for her and the baby. She learned that she would need to make some lifestyle changes for the remainder of her pregnancy to avoid the risks associated with high blood sugar levels.
– Treatment Plan:
- Oral medications (metformin) to help control blood sugar
- Regular blood sugar monitoring
- Lifestyle changes
At first, Rosa struggled with these changes. Many of the foods she loved, such as tortillas, rice, and sweets, were now restricted. Her doctor encouraged her to eat more vegetables, lean proteins, and whole grains. He also referred her to a nutritionist who helped her come up with meal plans that fit her tastes while keeping her blood sugar in check.
Complications:
The biggest concern for Maria and her doctors was the risk of macrosomia—the baby growing too large, which can complicate delivery. Additionally, there was a risk of **pre-eclampsia**, a condition that can cause high blood pressure and pose dangers during childbirth.
Maria was placed on a strict diet plan that focused on controlling carbohydrate intake. She had to avoid traditional foods like tortillas, sugary drinks, and pan dulce (sweet bread), which were a regular part of her meals. Initially, she struggled with the new diet, feeling deprived of her favorite foods, but she knew it was important for her baby’s health.
Despite her best efforts, Maria’s blood sugar levels remained elevated, and she eventually had to start insulin therapy. This was a new challenge for her, as she had to learn how to give herself injections and adjust her insulin dosage depending on her blood sugar readings. Her doctor assured her that this was a temporary measure and that most women with gestational diabetes return to normal after giving birth.
Complications:
- Increased risk of having a large baby (macrosomia)
- Higher likelihood of a cesarean section (C-section) due to baby’s size
- Risk of pre-eclampsia
- Higher chance of developing type 2 diabetes later in life
Cultural and Family Support:
Maria’s family was initially hesitant about the dietary changes, especially since food is such an important part of family life and celebrations. However, with her doctor’s guidance, Maria was able to adapt traditional Mexican dishes in ways that were healthier for her condition.
For instance, she swapped out traditional corn tortillas for whole wheat versions and reduced her portion sizes for carb-heavy dishes like **enchiladas** and **tamales**. She also learned to make lower-carb versions of **arroz con leche** (rice pudding) by substituting some of the ingredients to better control her blood sugar. Her husband and extended family began to support her by preparing meals with more vegetables and lean proteins, making it easier for her to stick to her new diet.
Delivery and Postpartum:
Maria’s careful management of her gestational diabetes paid off. She gave birth to a healthy baby boy at 38 weeks via a planned C-section due to his larger size (he weighed 9 pounds at birth). Thankfully, she did not develop pre-eclampsia, and both Maria and her baby were healthy after delivery.
After the birth, Maria’s blood sugar levels returned to normal, but her doctor warned her about the increased risk of developing type 2 diabetes in the future. She was encouraged to maintain a healthy diet and exercise regularly to lower that risk, and she continued to monitor her blood sugar periodically to ensure it stayed within a healthy range.
Life Today:
Maria is now an advocate for gestational diabetes awareness in her local community. She shares her story with other pregnant women, especially those who might not have easy access to healthcare or may not recognize the signs of gestational diabetes. She emphasizes the importance of early testing and close monitoring, as well as the need for a supportive family environment to make the necessary lifestyle changes.
Maria has remained committed to the healthy eating habits she adopted during pregnancy and is determined to stay proactive about her health to prevent type 2 diabetes from developing in the future.